Voices of Biotech
Podcast: MilliporeSigma says education vital to creating unbreakable chain for sustainability
MilliporeSigma discusses the importance of people, education, and the benefits of embracing discomfort to bolster sustainability efforts.
April 18, 2017
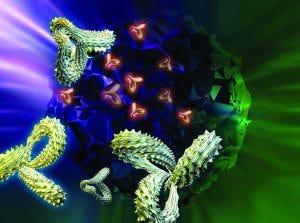
Protein structure is vital to function — and thus a critical parameter for determining biosimilarity. (STOCK.ADOBE.COM)
In a just a few years, the biopharmaceutical industry has gone from questioning the feasibility of “follow-on biologics” (around the time of BPI’s first issues) to fearing them (when we published our first supplement on the topic in 2013) to the acceptance and strategizing of today. Perhaps because of its more socialized medicine, Europe led the way in biosimilar regulation and approved its first such product nearly 10 years before the first US biosimilar launch in 2015. In between came 2009 approvals in Canada and Japan. And the World Health Organization adopted its own guidance in 2010 to encourage regulatory harmonization across markets.
Amgen is one innovator company that has embraced the concept wholeheartedly, calling it “our next chapter in healthcare” in a 2016 report (1). That publication cites product characterization, preclinical studies, nomenclature, reimbursement, and regulatory pathways as the primary challenges facing companies in biosimilar development. It also highlights the power of formulary decision makers, suggesting that they are likely to be more amenable to biosimilars with larger projected patient populations (e.g., anti–tumor necrosis factors, granulocyte-colony stimulating factors, erythropoiesis-stimulating agents, and interferons).
Technicalities
It’s true that biosimilars don’t face the same gauntlet of clinical testing that innovative biologics do. Generally, they can skip over phase 2 and go right from a large-scale phase 1 comparative pharmacokinetic/pharmacodynamic (PK/PD) and safety study right to large-scale comparative phase 3 trials. Data from testing just one indication may be extrapolated to others served by the comparator drug. Both of those options save developers substantial money, thus making it possible to sell biosimilars for lower prices than those of the innovator products.
However, that puts the onus on earlier testing — in particular, in vitro and animal testing as well as comparative characterization. At least three development batches are tested (fewer than for innovators, more than for generic drugs), and release testing remains a requirement. The Pharmaceutical Research and Manufacturers of America (PhRMA) estimates that development of a new biopharmaceutical may cost $2 billion over a decade or more; the Federal Trade Commission has estimated that biosimilar development could cost just $200 million over eight to 10 years.
A significant portion of that money is spent on product analysis. The Association for Accessible Medicines (AAM) claims that “there is a misconception that clinical trials will assure the safety of biosimilars, when instead, analytical comparisons will be the most powerful tool in determining whether a biosimilar is ‘highly similar’ to its reference product.”
When a biosimilar application is made, regulators will have had up to 20 years of history with its reference comparator. Prescribers will be familiar with clinical responses to that product, and it will have a documented adverse-event history. Meanwhile, the technology for evaluating the structure and function of biologics has improved over time.
Most adverse events for protein therapeutics are caused by their pharmacological properties or amplified drug effects. Contrary to public opinion, impurities do not cause adverse events for most biotech products. Purity is controlled to regulatory-defined levels and needs to be identified and controlled for biosimilars just as for any other medicine. Impurity differences (within specified limits) do not justify large clinical trials even if a biosimilar’s impurity profile may be different from its comparator’s. Preclinical testing (e.g., on animals and cells) should provide the necessary data.
As AAM points out, laboratory analyses can detect product differences more directly than clinical trials can. Modern analytical methods are more sensitive, precise, and reproducible than ever before. Functional assays confirm whether a biosimilar has the same activity as its reference originator. And after product approval, postmarket pharmacovigilance systems help companies monitor adverse events for years to come.
The box below describes just one of many analytical advancements that have helped companies realize the concept of well-characterized biologics in recent years. The many capabilities of mass spectrometry have made it an essential technology for every biopharmaceutical laboratory. Other valuable methods include high-performance liquid chromatography (HPLC), circular dicrhoism (CD), differential scanning calorimetry (DSC), light-scattering and electrophoretic technologies, analytical ultracentrifugation (AUC), and surface plasmon resonance (SPR) analysis.
Bioassays such as enzyme-linked immunosorbent assays (ELISAs) are just as important to biosimilar development as to innovators — and with the clinical testing differences, maybe even more so. Ulrike Herbrand provides much more detail on that in this report’s third article. And Bruno Speder follows with a focus on the biosimilar clinical development path.
“A sound understanding of a molecule, its mechanism of action (MoA), and potential impurities and degradation products during its production will assist a biosimilar applicant in discussions with regulatory authorities when considering safety and efficacy study designs” (2). Thus preclinical studies and characterization are the keys to opening the door of an investigational new drug (IND) application for clinical testing. Well worth revisiting, two recent BPI articles have examined the role of biophysical analysis and the orthogonal approach (3) and how to overcome challenges of highly concentrated biosimilar formulations (4). Gaps in science remain even for monoclonal antibodies (MAbs), which are by many accounts the most well-understood biopharmaceutical molecules — lending themselves to “platform” approaches to many operations (5).
Advancements in Characterizing Therapeutic Protein Higher-Order Structure by Mike Bogan and Henry Benner (IonDx, Inc.) |
Electrospray-ionization mass spectrometry (ESI-MS) is a well-established tool for biotherapeutic analysis. It draws intact proteins or peptide ions into the vacuum of a mass spectrometer, where the ion mass is measured. Electrospray ion-mobility mass spectrometry (ESI-IMS) introduces ions into a low-pressure gas, where the effects of aerodynamic drag reveal their shape. This technique is just emerging as a valuable tool for characterizing intact proteins, even though for a decade it’s been the basis of a commercially available medical diagnostic test that measures the size distributions of lipoproteins for cardiovascular risk assessment. A growing body of evidence shows that ion mobility provides critical information about intact antibodies, protein–protein interactions, and protein aggregation. It leverages some concepts behind ESI-MS (e.g., sensitivity, dynamic range, and reproducibility) but differs in that ESI-IMS measures protein shape directly and rapidly detects subtle changes in higher-order structure. It’s becoming a sensitive probe for protein conformation and can be used to characterize intact biotherapeutics, drug-conjugates, and nanoparticle–drug assemblies. Recently, IonDx has made key advances in the application of electrospray ion mobility to biotherapeutics. Our new protein characterization platform for biologics is based on improvements to several ion-mobility technologies. Our patented technology combines electrospray ionization with improved ion optics and detection, eliminates charge distortion typically encountered with highly-charged electrospray ions, and introduces a new way to quantify variations in the shape of biotherapeutic molecules. One promising application for ESI-IMS is to generate biophysical “fingerprints” for comparing biosimilars with innovator drugs. As more of the latter fall off patent, the former continue to increase in number. Regulators require biosimilars to exhibit biophysical fingerprints that are comparable to the innovator drugs they are meant to replace. With increasing emphasis on analytical data for biosimilar characterization, John Jenkins (director of the Office of New Drugs at the US FDA) suggests that applicants develop new and innovative approaches for studying their products. Fingerprints help establish comparability, according to recently released guidances (2, 3). Interchangeability also can be demonstrated with fingerprints, but some are better than others. Key to generating a biophysical fingerprint of higher-order structure using ESI-IMS is to analyze singly charged ions rather than the typical highly charged antibodies measured by native MS. To do so, we reduce the net charge on electrosprayed droplets to a single charge. Eliminating high charge states prevents them from stretching a protein in the gas phase and simplifies data interpretation by eliminating the need to deconvolute charge states. We have overcome these challenges by developing a standalone ion-mobility spectrometer with patented detector technology suitable for measuring the ion mobility of singly charged macromolecular ions. Historically, a protein’s three-dimensional structure has been determined with methodologies developed by the X-ray crystallography community. Indeed, their techniques serve as the gold standard against which other techniques are contrasted. But X-ray crystallography captures only a single protein structure. If a protein has more than one structure, or its uncrystallized form varies, those variations are not revealed. Thus, less-precise but faster techniques for determining protein structure are relied upon increasingly — even if they provide only an indirect measurement of protein structure. Our technology measures ion shape both directly and rapidly. Mike Bogan is director of development, and Henry Benner is founder and CEO of IonDx, Inc., 8 Harris Court C5-6, Monterey CA 93940; www.iondx.com. |
Regulatory Affairs
Our 2013 supplement was full of questions, many of which have been answered. Since 2015, the US Food and Drug Administration (FDA) has published five guidances related to biosimilar development (6–10). Now it’s all about interpretation. Three of those five documents involve the characterization and comparison issues described above. One focuses on nomenclature, the last on meetings between applicants and the agency.
The Alliance for Safe Biologic Medicines surveyed hundreds of healthcare providers in 2015, discovering that 80% of physicians and 76% of pharmacists want information in biosimilar product labels to specify for which indications they actually were studied (rather than extrapolated from other testing). Regulators around the world currently disagree on whether a biosimilar tested for one indication can be used for other indications that its comparator is used to treat. For example, the European Medicines Agency allows for full extrapolation, Health Canada specifies classes of disease that go together, and the FDA has yet to finalize its policy.
Every article in this report discusses regulatory aspects of biosimilar development. Ron Rader wraps things up at the end by looking at things from a global perspective, with a special focus on product names. Rader has been BPI’s “go-to” guy for nomenclature issues ever since he first brought them to our awareness back in 2007, before he joined BioPlan Associates (11–12).
A Wide-Open Market Beckons
Amgen is considering the following questions when it comes to the future of biosimilars (1): How will payers respond to their launch? How will pharmacy benefit managers influence uptake in the biosimilar market, and will market uptake reflect factors beyond cost savings? How will appropriate use in therapy evolve as different stakeholders become familiar with biosimilars? How will nomenclature be determined, and what are the ramifications? And how will stakeholders value factors related to reimbursement?
Clearly, market considerations are on everyone’s mind. So are regulations — especially in the United Kingdom (which since Brexit is severing its laws from those of the European Union) and the United States (where uncertainty suddenly has become the order of the day). How much of the EU approach will remain in the UK regulatory system? What would a new US paradigm of eliminating two regulations for every new one introduced mean for how regulated industry functions? And what will Tom Price’s influence be like on the Department of Health and Human Affairs (not to mention Seema Verma’s on Medicare and Medicaid)? All that remains to be seen — but for now, we must operate on the information we have rather than speculating on what may come.
A 2016 report from Industry Standard Research claims that nearly two out of three survey respondents said their companies were planning to sell biosimilars — a significant increase from one out of two in 2015 (13). The market at this point is wide open. Early adopters may have a head start, but the real winners will be those who can address and overcome the technical difficulties.
Outsourcing Can Help |
Many contract testing, research, and manufacturing/development organizations offer biosimilar expertise. Some such companies were reluctant to publicize that fact just a few years ago — for fear of alienating their innovator clients — but those concerns seem to have lessened as of late. |
Contract Testing Organizations (CTOs): With characterization and preclinical testing increasing in importance for the biosimilar era, it’s no surprise that a growing number of specialized laboratories are offering such expertise as a service. Charles River Laboratories and SGS are represented elsewhere in the pages of this special insert. Others include BioAgilytix, Creative Proteomics, Eurofins Scientific, Intertek, Myoderm (which specializes in obtaining innovator materials for comparative testing), and SSCI. |
Contract Research Organizations (CROs): CROs can be distinguished from CTOs in that they typically focus on managing clinical trials. Quintiles IMS and Parexel are perhaps the biggest names here. Others include Altasciences, IDDI, INC Research, inVentiv Health, and Pharmaceutical Product Development (PPD). |
Contract Manufacturers and Development Organizations (CMOs/CDMOs): Never before has the concept of a “virtual company” been more feasible in the biopharmaceutical industry. As CMOs are evolving into CDMOs, some are adding biosimilar development to their portfolios. Early adopters include Boehringer Ingelheim and Laureate Biopharmaceutical Services (now part of Gallus BioPharmaceutical), both of which participated in BPI’s 2013 biosimilars supplement. Others betting on biosimilars include Samsung BioLogics and Celltrion. And after the SAFC/Millipore merger, strategic alliances (e.g., with Turkish biosimilars company Turgut Ilaç in late 2015) allow MilliporeSigma to offer Provantage end-to-end development and manufacturing of biosimilars. Some outsourcing companies offer their own proprietary technologies for licensing along with associated services. For example, ProBioGen touts both its expertise in development of biosimilars and biobetters and its innovative technologies related to chemically defined media and yield enhancement, immunogenicity testing and bioassays, and antibody–drug conjugation. Lonza has specialized culture media and cell lines. As the biosimilar arm of Novartis, Sandoz develops its own products as well as providing contract services. Similarly, Curaxys is a Spanish company that develops its own generics and biosimilars but also provides contract manufacturing and development services. |
References
1 Adamson R, et al. 2016 Trends in Biosimilars Report. Amgen Inc.: Thousand Oaks, CA, 2016.
2 Dinwoodie N. Outsourcing Biosimilars Development. BioProcess Int. 14(5) 2016: S30–S35.
3 Greer FM. Primary and Higher-Order Structural Characterization Strategy for Biosimilarity Assessment. BioProcess Int. 13(11) 2015: 40–44.
4 Qi W, et al. Enhanced Biosimilar Product Characterization: A Case Study Using Raman Spectroscopy Combined with Dynamic Light Scattering. BioProcess Int. 14(6) 2016: 44–49.
5 Kaur SJ, et al. Biosimilar Therapeutic Monoclonal Antibodies: Gaps in Science Limit Development of an Industry Standard for Their Regulatory Approval (Parts 1 and 2). BioProcess Int. 14(9) 2016: 12–21; 14(10) 2016: 22–27.
6 CDER/CBER. Quality Considerations in Demonstrating Biosimilarity of a Therapeutic Protein Product to a Reference Product: Guidance for Industry. US Food and Drug Administration: Rockville, MD, April 2015.
7 CDER/CBER. Scientific Considerations in Demonstrating Biosimilarity to a Reference Product: Guidance for Industry. US Food and Drug Administration: Rockville, MD, April 2015.
8 CDER/CBER. Formal Meetings Between the FDA and Biosimilar Biological Product Sponsors or Applicants: Guidance for Industry. US Food and Drug Administration: Rockville, MD, November 2015.
9 CDER/CBER. Considerations in Demonstrating Interchangeability with a Reference Product: Guidance for Industry. US Food and Drug Administration: Rockville, MD, January 2017.
10 CDER/CBER. Nonproprietary Naming of Biological Products: Guidance for Industry. US Food and Drug Administration: Rockville, MD, January 2017.
11 Rader RA. What Is a Generic Biopharmaceutical? Biogeneric? Follow-On Protein? Biosimilar? Follow-On Biologic? (Parts 1 and 2) BioProcess Int. 5(3) 2007: 28–38; BioProcess Int. 5(5) 2007: 20–28.
12 Rader RA. Nomenclature of New Biosimilars Will Be Highly Controversial. BioProcess Int. 9(6) 2011: 26–33.
13 Bioprocessing Manufacturing: Key Considerations and Expected Outsourcing Practices (3rd Edition). ISR Reports: Cary, NC, May 2016.
Cheryl Scott is cofounder and senior technical editor of BioProcess International, PO Box 70, Dexter, OR 97431; 1-646-957-8879; [email protected]; www.bioprocessintl.com.
You May Also Like