A Theradaptive scientist works with a three-dimensionally printed construct that will carry material-binding therapeutic proteins for bone-tissue regeneration.
In March 2023, I took the opportunity to speak with Luis Alvarez about the founding of Theradaptive. The company specializes in engineering recombinant proteins, with an initial focus on developing therapeutics for regeneration of soft, vascular, and bone tissue. “Theradaptive grew out of my thinking about combat injuries,” Alvarez told me. Before earning a doctoral degree in biomedical engineering from the Massachusetts Institute of Technology and working as cofounding deputy director of the US Department of Defense’s regenerative medicine program, he served in the US Army during the Iraq War.
Alvarez witnessed severe injuries during his tour. “When I returned from Iraq,” he continued, “I spoke with friends who were physicians at the Walter Reed National Military Medical Center in Bethesda, MD. They told me about their experiences in performing delayed amputation.” Essentially, a patient sustains a severe injury to an extremity, and despite — sometimes multiple — medical interventions, the bone does not heal correctly in the coming weeks or months. Then, the limb must be removed, and the patient is fitted for a prosthetic. “I believed that delayed amputation was a ‘medieval’ problem to have in modern medicine,” Alvarez said. He requested reassignment to graduate studies at MIT as well as a change in designation from military intelligence to research and development (R&D). “So I went to MIT and focused on the problem of targeted tissue regeneration.”
Depending on the type and severity of tissue injury, several regeneration approaches are possible. For instance, growth factors have been applied to modulate immune responses and encourage cellular movement to damaged tissues (1). By and large, however, biopharmaceutical companies have focused on cell-based interventions, especially for treatment of traumatic injuries. Stem cells derived from bone marrow, adipose tissue, and skin all have shown promise in effecting angiogenesis and modulating immune responses to establish favorable conditions for tissue growth (2, 3). Pharmaceutical and medical-device developers also are experimenting with implantable biomaterials (1, 4, 5). Those include tissue grafts made from electrospun collagen nanofibers. Chitosan has been used as a scaffold for growth factors and stem cells. And decellularized matrices have been developed to promote infiltration of patient cells at the site of injury. Thus, Theradaptive’s work with therapeutic proteins and biodevices represents a novel intervention in regenerative medicine.
I asked Alvarez about why recombinant proteins have been difficult to apply in regenerative medicine — and why that application is still worth pursuing. He highlighted traditional limitations on biologic delivery and bioavailability, then described how his company uses computational engineering to identify “material-binding variants” of native proteins that adhere to implantable substrates. Those variants enable targeted therapy delivery, facilitating regeneration of severely damaged tissues.
 Protein-Delivery Problems
Protein-Delivery Problems
Why haven’t therapeutic proteins received as much consideration in the regenerative-medicine space as stem cells and other such interventions? Clearly, proteins play an important role in tissue regeneration. But when they initiate the cell signaling required for that process, they are acting on cells that are already in a patient’s body. In many cases of serious tissue injury, the problem is not a lack of cells, but an inability to control protein delivery to the locations and over the durations that are needed to effect tissue repair. That has been more challenging than, say, isolating and/or culturing cells and injecting them into a target tissue. Although cells are highly complex products, delivering them is easier than it is to place proteins and keep them where they are needed.
Proteins diffuse easily. Upon administration, they can dissipate from the site of injection over minutes to hours depending on how large they are. But most of the biological processes implicated in tissue regeneration require an elevated protein presence for days to weeks or, in some cases, months. The field of regenerative medicine generally has been unable to sustain that level of protein activity and availability.
What strategies have drug developers used to deliver therapeutic proteins to injury sites, and how does your company’s approach differ? The field usually has experimented with encapsulation and/or mechanisms for timed release. The rationale is that meting out proteins slowly will help to produce the intended effect. In some cases, that strategy can work, but a major limitation is that, at any given time during treatment, most of the therapeutic dose is unavailable to the damaged tissues. Much of the protein content is encapsulated (and thus inactive) until it is released.
Our approach is to set therapeutic proteins on the surface of an implanted material, whether that is a particle, injectable slurry, or hardware device. Thus, an entire therapeutic dose is made available to cells from day zero, and they can interact with the surface material because of its bioactivity. That feature is important: Surface-area interactions influence how bodies regenerate tissue and initiate immune responses.
How does your company ensure that therapeutic proteins adhere to the implanted material? We use protein-engineering technologies to identify variants of established therapeutics. Those variants are designed to bind tightly with carrier material without compromising their biological activity. For instance, our most mature development program is for spinal fusion and orthopedic repair. We subjected native bone morphogenetic protein 2 (BMP2) — which we know makes bone well but does not bind effectively with carriers — to our engineering process. We ultimately produced and patented a variant that we call AMP2 protein. It can be loaded easily onto a carrier for surgical implantation.
Engineering Protein Variants
How difficult is the protein-engineering process? Generally, it is very difficult. I don’t mean to discourage other companies from doing it because it is now possible to perform it in a clinically meaningful way. But it’s not a weekend job.
The type of protein engineering that we perform is like looking for a needle in the proverbial haystack. You are searching for a sequence that will mediate a strong binding interaction to a given material. Unless you know from first principles how to make that sequence, you basically need to search through a large library. That’s what we do: We search large sequence libraries to identify promising variants of proteins with proven therapeutic effects. We do some in silico enhancement of candidate sequences, then refine those designs again and again in a kind of repeated evolution to achieve a stable protein that expresses well and binds tightly to the material of interest.
We have developed an in-house bioinformatics resource that lets us modify promising protein sequences from in vitro screens. Then we can design variants that are oriented “rationally” toward the needed characteristics without destroying the beneficial properties that the original screens highlighted. Instead of creating an additional, highly diverse library, we’re compiling a “biased” library that is informed by what we know about screened proteins.
What biophysical characteristics do you pay the most attention to when you’re engineering protein variants? We start with proteins that have produced a given biological effect during animal and even human studies. The protein also should be amenable to recombinant production. Even then, of course, we are left with a broad subset of therapeutic proteins. Otherwise, we face no restrictions because we determine everything else about our proteins in silico. Can a particular protein be modified using our method without interfering with its biological function? That’s true for 98% of proteins in our library. Nearly every protein has “real estate” that can be modified without interfering with its receptor interaction.
 Material Concerns
Material Concerns
How would you describe a typical workflow for adhering protein variants to a carrier? Consider our implant for effecting spinal fusion. Because our therapeutic proteins already encode the genetic modifications needed for adherence to the carrier material, no other processing is required. The implant is dipped into a liquid formulation of the protein product. After 10 minutes, the device is fully coated. The proteins behave almost like a paint on the carrier material such that the surface-displayed molecules show full bioactivity.
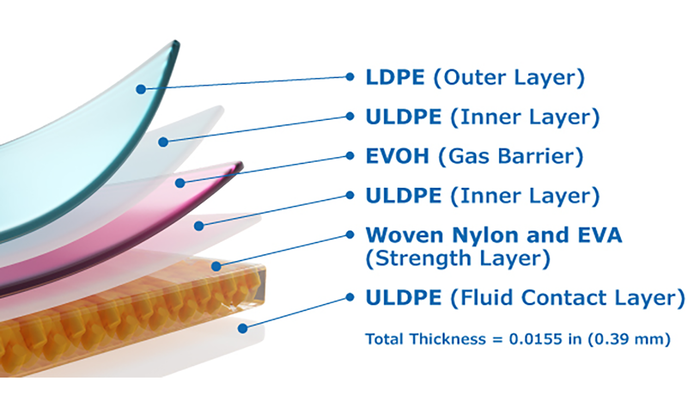
Are particular materials more or less difficult to work with? And once proteins have adhered with a carrier, does the resulting biodevice have special storage requirements? Polytetrafluoroethylenes (PTFEs) and some highly inert polymers do not bind easily with anything, so such materials are not well suited to our process. But most implantable materials are easy for us to work with, including metals, inorganic materials, injectable ceramics, and resorbable polymers.
The nice thing about binding proteins to carriers is that doing so creates good conditions for stability. The proteins that we have worked with generally have been highly stable, and we can store the resulting biodevices at room temperature without significant limitations on duration. For some products, we even can perform terminal sterilization. Typically, a protein drug product is formulated in a solution phase. Under such conditions, terminal sterilization would destroy the therapeutic proteins. We have shown that we can preserve our proteins throughout sterilization, so we also can perform aseptic manufacturing of combination products. Surface tethering raises several significant benefits for protein stability.
Future Applications
What are you learning as Theradaptive’s technology moves into clinical trials? Our most mature program uses our AMP2 product for spinal fusion and orthopedic repair more generally. That includes dental, nasal, facial, and other bone tissues. We have completed preclinical work for that program, outperforming the standard of care in each study. We will start clinical trials for the spinal-fusion indication later in 2023.
We are applying lessons from those studies to our next program, which addresses an oncology indication. We are tethering an immunomodulatory molecule onto a carrier that can be injected near or within a tumor to raise an immunostimulatory signal. That approach would circumvent the problems of systemic administration. Exposing an entire body to an immunostimulatory agent generates multiple side effects.
As with our first program, our goal is to leverage precise placement of a drug. That possibility is highly relevant for oncology applications. Many previously developed cancer therapies have been formulated for systemic administration. We can apply our methods to reengineer such proteins and transform them into variants for local delivery. To that end, we are seeking to collaborate with other drug developers and manufacturers.
References
1 Pang C, et al. An Overview of the Therapeutic Potential of Regenerative Medicine in Cutaneous Wound Healing. Int. Wound J. 14(3) 2017: 450–459.
2 Thurairajah K, Broadhead ML, Balogh ZJ. Trauma and Stem Cells: Biology and Potential Therapeutic Implications. Int. J. Mol. Sci. 18(3) 2017: 577.
3 Wang Y, Pati S, Schreiber M. Cellular Therapies and Stem Cell Applications in Trauma. Amer. J. Surg. 215(5) 2018: 963–972.
4 Brovold M, et al. Naturally-Derived Biomaterials for Tissue Engineering Applications. Novel Biomaterials for Regenerative Medicine. Chun HJ, et al., Eds. Springer: Singapore, 2018: 421–449.
5 Sharma K, Mujawar MA, Kaushik A. State-of-Art Functional Biomaterials for Tissue Engineering. Front. Mater. 6, 2019.
Brian Gazaille is managing editor of BioProcess International; [email protected].