The Next Frontier for Viral-Vector Vaccines: Considerations for Manufacturing and OperationsThe Next Frontier for Viral-Vector Vaccines: Considerations for Manufacturing and Operations

2,000-L bioreactor and associated control system for production of viral vectors at the ReiThera facility in Rome, Italy (HTTPS://REITHERA.COM)
Viral vectors continue to generate considerable excitement in the biopharmaceutical industry, albeit primarily for advanced-therapy applications. The BPI editorial team receives multiple manuscripts each year relating to production, purification, and formulation of adenoassociated virus (AAV) and lentivirus (LV) vectors for in vivo delivery of gene therapies and ex vivo modification of patient/donor cells, respectively. Compared with such applications, viral-vector vaccines receive far less attention; however, they merit serious consideration because they hold much promise for mitigating infectious diseases.
Viral-vector vaccines are not entirely new technologies. The first use of a viral vector to express a foreign gene goes back to 1972, when Jackson et al. used simian virus (SV) 40 to carry genes from enterobacteria phage λ and Escherichia coli (1). In 1984, Moss et al. reported their development of a hepatitis B vaccine for chimpanzees based on live recombinant vaccinia virus (2). Researchers have since investigated many vector types, including different strains of adenovirus (Ad), alphavirus, flavivirus, herpesvirus, paramyxovirus, poxvirus, and rhabdovirus (see “Viral Vectors” box) (3). Although veterinary applications are proliferating (4), viral-vector vaccines for humans have experienced little uptake among drug companies — except during public-health emergencies.
During the West African Ebola virus epidemic of 2013–2016, for example, enthusiasm grew for viral vectors as researchers investigated recombinant vesicular stomatitis virus (VSV), Ad, and other such vehicles for antigen-gene delivery. A similar surge in interest occurred early in the COVID-19 pandemic as viral vectors emerged alongside messenger RNA (mRNA) as viable vaccine approaches. Globally, several vector-based candidates advanced rapidly into clinical evaluation. Some such vaccines even received emergency authorization and/or regulatory approval in specific regions, including Ad-based candidates developed by AstraZeneca–Oxford University (United Kingdom), Bharat Biotech (India), CanSino (China), and Janssen–Johnson & Johnson (J&J, United States). Those products represent significant scientific achievements. As of December 2022, Janssen–J&J’s Jcovden vaccine against SARS-CoV-2 remains the only viral-vector vaccine to have received emergency-use authorization (EUA) from the US Food and Drug Administration (FDA), and no such vaccines have gained full approval (5). However, the regulatory and commercial successes of Pfizer–BioNTech’s and Moderna’s respective mRNA vaccines seem to have dampened enthusiasm for viral-vector approaches, as have rare safety concerns associated with J&J’s and AstraZeneca’s respective products (6, 7).
Still, some companies have persisted in their efforts to bring viral-vector vaccines into clinical trials and commercialization. One such company is ReiThera Srl, a contract development and manufacturing organization (CDMO) based in Rome, Italy. With deep roots in vaccine development, the company now works with multiple vector types to support production of prophylactic and therapeutic products. For instance, ReiThera manufactured drug substance and performed fill–finish activities for the Sabin Vaccine Institute’s Ebola vaccine, which uses vectors based on chimpanzee adenovirus (ChAd) serotype 3. By January 2023, 9,600 doses will have been delivered, with support from the World Health Organization (WHO), to help mitigate the current epidemic in Uganda. Another 25,000 doses will be manufactured on a rolling basis early in 2023 (8).
At the end of 2022, I spoke with Stefano Colloca, ReiThera’s chief technology officer, to learn about what innovations are needed to advance viral-vector vaccines into commercial manufacturing. Colloca provided insight into the potential value of viral-vector vaccine approaches, especially for prevention of infectious disease. Highlighting the breadth of available vector technologies, he also explained what capabilities companies must have if they are to undertake multiple viral-vector programs.
Before serving in his current role, Colloca cofounded and directed viral-vector programs at Okairos Srl, the company from which ReiThera spun out in 2014. He also has worked as a senior research fellow at Italy’s Istituto di Ricerche di Biologia Molecolare (IRBM), where he contributed to drug-discovery programs for hepatitis B and C viruses (HBV, HCV) and development activities for Ad-based vaccines.
The Value of Viral-Vector Approaches
What experience does your company have with producing viral-vector vaccines? ReiThera began as a company called Okairos, which itself had spun out of Merck & Co. Our team specialized in developing genetic vaccines for major infectious diseases. For instance, we worked on a vaccine for HCV. At the time, vaccine approaches for that indication often used Ad serotype 5, but that vector is highly seroprevalent in humans, especially in young people. We worked with alternative serotypes and developed a platform technology based on ChAd vectors. Merck ultimately decided to continue working with human Ad systems, so under a technology-licensing agreement, we formed Okairos to advance the ChAd platform for different vaccine applications.
As Okairos, we developed vaccines against several diseases. One of our original products was a vaccine against the Sudan Ebola strain, which we developed in collaboration with the US National Institutes of Health (NIH). Now, that candidate is under evaluation by the WHO, with clinical trials taking place in Uganda. The candidate is based on ChAd3 vectors. We also developed vaccines for HCV, respiratory syncytial virus (RSV), malaria, rabies, and other infectious diseases.
GlaxoSmithKline (GSK) acquired the intellectual property and vaccine-development capabilities of Okairos in 2014. Since rebranding as ReiThera, we have served as a CDMO specializing in viral-vector products. We continued to collaborate with GSK on three vaccine programs until the end of 2020, after which our company was independent and free to operate. We still retain links to our Ad vector technology, and we have continued to develop some viral-vector products such as a SARS-CoV-2 vaccine based on a gorilla Ad system. We ushered that program into phase 2 clinical trials.
During the COVID-19 pandemic, mRNA vaccines received more attention than those based on Ad and other viral vectors. In what contexts might viral-vector vaccine delivery be particularly valuable? Interest in Ad dropped after reports of blood-clotting side effects from vaccines based on the Oxford University–AstraZeneca ChAdOx1 vector (7). Therefore, Ad is unlikely to be an attractive option for pandemic-vaccine development. However, it will remain an important technology for other applications.
Several studies of COVID-19 vaccines have demonstrated the superiority of Ad vectors over mRNA in stimulating T-cell responses, which are important not for inducing sterilizing immunity, but for preventing severe disease. I believe that Ad-based vaccines will play a critical role in treating cancers and infectious diseases. For instance, recent publications have proposed using an immunization strategy based on Ad and modified vaccinia Ankara (MVA) vectors to complement antiretroviral therapies for HIV-positive individuals (9). In addition to exploiting Ad’s ability to stimulate T-cell responses, drug developers can leverage the vector’s aptitude for transient gene delivery and expression.
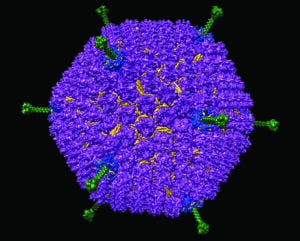
Despite the enthusiasm surrounding mRNA, vaccines based on viral vectors such as human adenovirus serotype D26, illustrated here, also are poised to become important tools for treating infectious disease. (VICTOR PADILLA-SANCHEZ, HTTP://DOI.ORG/10.5281/ZENODO.5132873)
What capabilities has your company needed to develop to manufacture Ad and other vectors at scale? We continue to work with several different vectors, and our service offerings are broad in scope. We work with customers starting from process and technology development and into phase 1 clinical trials, phase 2 process validation, and even commercial manufacturing. We have the breadth of expertise and now the manufacturing capacity to accommodate market demand. For Ad-based products, our capacity ranges from milliliter-level processes in shake flasks up to 2,000-L stirred-tank bioreactors, which represent the industry standard for production. We can work not only with suspension-culture technologies, but also with adherent cells grown in fixed-bed bioreactors.
Initially, our facility housed 870 m2 of space for current good manufacturing practice (CGMP) production suites, 170 m2 for a quality control (QC) laboratory, and more than 700 m2 for research and GMP support. The latter section contains a filling suite equipped with an open restricted-access barrier system (oRABS) isolator with a fully automated aseptic-filling machine validated for batch sizes of 3,500 vials (2R, 6R, and 10R types). In November 2022, the Italian Medicines Agency (AIFA) also authorized operations in a new 1,500-m2 production area dedicated to large-scale processes. Therein, we can work with 200-L to 2,000-L suspension bioreactors. We are equipped to perform perfusion cultures to increase cell densities, and we have developed a culture process at high cell density for Ad vectors. Our aim with that process is to increase productivity and yield such that at least one dose can be obtained from each milliliter of cell culture.
Although our expertise historically lies in Ad production, we also work with vectors such as MVA. That virus can be difficult to produce for different reasons. Because it is relatively large, products based on it cannot be sterilized by filtration. Instead, processes must be aseptic. MVA-based products also require continuous production and use a potentially tumorigenic cell line. Thus, we have needed to develop a downstream purification process that reduces residual impurities well beyond levels that regulators have deemed to be acceptable in other drug products (10). We already have produced and released for clinical use several batches of MVA using suspension and adherent culture processes.
Another vector technology in our portfolio is herpes simplex virus (HSV) type 1, which like MVA raises difficulties because of its large size, necessitating aseptic processing. We also work with AAV, which today is considered to be the most important vector in the field of gene delivery. Most of the companies developing AAV products are focused on either rare genetic diseases, treatments that require substantial vector doses, or ocular diseases, for which small vector quantities might be sufficient to achieve a therapeutic effect.
Here, the next frontier is scale-up. Manufacturers still are figuring out how to transfer a small-scale process (e.g., for production of clinical-trial supply or commercial manufacturing of a niche therapy) to larger scales for indications that require high vector quantities. For instance, therapies targeting large organs need much higher vector quantities than do ophthalmic treatments.
A couple of options are possible. At ReiThera, we have developed a process for transient transfection of AAV in suspension-adapted cells. That process is ready for application, and we are working with different companies to produce clinical lots based upon it. A more innovative method to produce AAV is to use a stable producer cell line that effectively eliminates transfection steps. We are developing such a process. Although it remains in development, preliminary results have been promising. We hope to offer the method to customers as soon as possible.
What does your company do to ensure that it can work with all of those vector types safely and effectively at the same campus? Our facility design makes that possible. Production occurs in different rooms with completely independent heating, ventilation, and air conditioning (HVAC) systems. We also have established a number of internal practices to prevent cross-contamination across different parts of the site. Essentially, we operate in a multiproduct facility, in which structural and procedural measures enable production processes to be run in parallel.
Which of the vector systems that you noted presents the greatest difficulties for manufacturing campaigns? Viral vector manufacturing is generally difficult because the production processes involved are complex. For instance, viral vector production implies use of a host cell line as well as the intended vector, which is a complex particle in and of itself. The most difficult aspect here is to ensure lot-to-lot consistency. You must establish a production process such that it generates consistent results.
That said, the field understands Ad vector biology quite well. Starting with Frank Graham’s studies of Ad transformation in the 1970s (11, 12) and his team’s subsequent development of the human embryonic kidney (HEK)293 cell line (13), we have developed a thorough account of the vector, including its stability upon virus replication. We know that transgene expression can interfere with Ad vector production. Thus, researchers have developed a cell line that shuts off transgene expression during Ad’s production phase. That approach increases both process productivity and vector stability. In many ways, Ad is, as a former colleague of mine put it, “a piece of cake.”
We have much to learn about other vector systems, each of which has distinct biological characteristics. For example, Ad replication occurs in a host cell’s nucleus, whereas MVA replication is cytoplasmic (10). Thus, you cannot apply the same production and recovery methods for those two vector types. For AAV, the production process is relatively simple but still problematic, requiring transfection of host cells and then vector harvest and purification. Scale-up is the traditional problem here. The goal is to manufacture a vector lot with good potency, a low level of empty capsids, and a good ratio between total genomes and infectious units.
You mentioned vector purification and recovery. What factors make purification of Ad and other viral vectors more difficult than, say, downstream processing of an mRNA-based product? Because mRNA can be produced without cells by in vitro transcription (chemical synthesis), both upstream and downstream processes are much simpler than those of viral vectors. The major challenge with vector purification is to eliminate process residuals, primarily but not only impurities from infected host cells. That can be achieved by a combination of methods, including depth/tangential-flow filtration and chromatography. However, one purification strategy cannot be generalized across different vector types.
For example, AAV appears in about a dozen different serotypes (including synthetic variants), each of which has distinctive properties that must be considered during downstream process development. The same goes for Ad and its serotypes. Regardless of the strategy applied, the goal is to reduce process residuals as much as possible without destroying virus particles. Infectivity must be maintained at a sufficiently high level to help ensure product potency.
As with other biopharmaceutical modalities, aggregation potential should be considered. Some viral vectors have a higher tendency to aggregate than others have, and that phenomenon can diminish product potency and stability. Drug-product formulation also needs to be customized for each vector. You cannot rely on a single formulation for all Ad products; a formulation must be adapted to each specific serotype. Essentially, the challenge is to find separation and formulation methods that leave a drug product sufficiently pure and stable without having a negative impact on vector quality.
BAs occurred with monoclonal antibody (MAb) production in the 1990s and 2000s, manufacturing of viral-vector vaccines is maturing. Some such products already have reached the market, often for niche applications. The current goal is scale-up, establishing production methods that can yield large quantities while meeting industrial standards. That objective is important for all vector platforms such as AAV and lentivirus (LV), even if the latter is often applied ex vivo — e.g., to generate chimeric antigen receptor (CAR) T-cell therapies — and thus does not need to be manufactured at massive scales. AAVs must be produced at large scales for future therapeutic applications — not only for ocular gene therapies, but also for drugs that target larger organs. Considerable effort is being directed into scale-up.
Most companies exerting such effort are still demonstrating proof of concept. The thinking generally has been that it doesn’t matter how we produce a vector candidate; for instance, let’s test our vector in animal models and then in clinical trials to demonstrate that our approach can succeed. But now such companies are trying to solve the manufacturing part of the equation. That has created a developmental bottleneck.
What strategies might alleviate that bottleneck? Viral-vector specialists can expand what they know about biomanufacturing using methods (e.g., suspension cell culture) that were developed for smaller biological modalities. Some companies are trying to eliminate transient transfection steps from the production stage. Doing so could facilitate vector production processes and increase their productivity. I don’t know whether manufacturing costs would decrease when using that strategy because starting materials (e.g., stable producer cell lines) still would need to be produced at GMP grade. But at least we would not need to deal with scaling up transfection.
What is next for your company? ReiThera is both a contract manufacturer and a viral-vector technology developer. We are working on another such technology that can be used for different applications, and we are keen to collaborate with companies that want to develop new therapeutic approaches. We continue to work on a transfection-free AAV production system and a large-scale process based on suspension bioreactors.
References
1 Jackson DA, et al. Biochemical Method for Inserting New Genetic Information into DNA of Simian Virus 40: Circular SV40 DNA Molecules Containing Lambda Phage Genes and the Galactose Operon of Escherichia coli. Proc. Natl Acad. Sci. USA 69(10) 1972: 2904–2909; https://doi.org/10.1073/pnas.69.10.2904.
2 Moss B, et al. Live Recombinant Vaccinia Virus Protects Chimpanzees Against Hepatitis B. Nature 311(5981) 1984: 67–69; https://doi.org/10.1038/311067a0.
3 Vrba SM, et al. Development and Applications of Viral Vectored Vaccines To Combat Zoonotic and Emerging Public Health Threats. Vaccines 8, 2020: 680; http://dx.doi.org/10.3390/vaccines8040680.
4 Baron MD, Iqbal M, Nair V. Recent Advances in Viral Vectors in Veterinary Vaccinology. Curr. Opin. Virol. 29, 2018; https://doi.org/10.1016/j.coviro.2018.02.002.
5 Viral Vector Vaccines. Infectious Diseases Society of America, 1 November 2022; https://www.idsociety.org/covid-19-real-time-learning-network/vaccines/covid-19-viral-vector-vaccines.
6 Safety Monitoring of the Janssen (Johnson & Johnson) COVID-19 Vaccine. US Centers for Disease Control and Prevention: Atlanta, GA, 7 May 2021; https://www.cdc.gov/mmwr/volumes/70/wr/mm7018e2.htm?s.
7 AstraZeneca’s COVID-19 Vaccine: EMA Finds Possible Link to Very Rare Cases of Unusual Blood Clots with Low Blood Platelets. European Medicines Agency: Amsterdam, The Netherlands, 7 April 2021; https://www.ema.europa.eu/en/news/astrazenecas-covid-19-vaccine-ema-finds-possible-link-very-rare-cases-unusual-blood-clots-low-blood.
8 Nelson M. ReiThera Supports Sabin’s Ebola Sudan Vax Production. BioProcess Insider, 21 December 2022; https://bioprocessintl.com/bioprocess-insider/deal-making/reithera-supports-sabins-ebola-sudan-vax-production.
9 Chen Z, Julg B. Therapeutic Vaccines for the Treatment of HIV. Transl. Res. 223, 2020: 61–75; https://doi.org/10.1016/j.trsl.2020.04.008.
10 Pavot V, et al. Generation and Production of Modified Vaccinia Virus Ankara (MVA) as a Viral Vector. Recombinant Virus Vaccines. Ferran M, Skuse G, Eds. Humana Press: New York, NY, 2017: 97–119; https://doi.org/10.1007/978-1-4939-6869-5_6.
11 Graham FL, van der Eb AJ. A New Technique for the Assay of Infectivity of Human Adenovirus 5 DNA. Virology 52(2) 1973: 456–467; https://doi.org/10.1016/0042-6822(73)90341-3.
12 Graham FL, van der Eb AJ, Heijneker JL. Size and Location of the Transforming Region in Human Adenovirus Type 5 DNA. Nature 251(5477) 1974: 687–691; https://doi.org/10.1038/251687a0.
13 Graham FL, et al. Characteristics of a Human Cell Line Transformed By DNA from Human Adenovirus Type 5. J. Gen. Virol. 36(1) 1977: 59–72; https://doi.org/10.1099/0022-1317-36-1-59.
Brian Gazaille, PhD, is managing editor of BioProcess International; [email protected]. Stefano Colloca, PhD, is chief technology officer and cofounder of ReiThera, Via di Castel Romano 100, 00128, Rome, Italy; [email protected].
You May Also Like






