3D Bioprinting Possibilities and Challenges3D Bioprinting Possibilities and Challenges
February 13, 2017
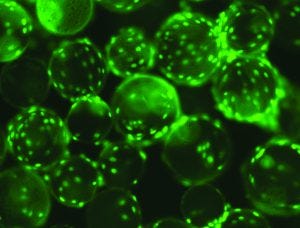
Human mesenchymal stem cells (hMSCs) on Corning Synthemax II polystyrene microcarriers (WWW.CORNING.COM)
Three-dimensional (3D) bioprinting is the newest addition to the regenerative medicine family. Now within the industry dedicated to providing more personalized drug products, this new additive-manufacturing technology has the potential to truly focus on individual tissue repair and replacement. In a short period of time, 3D bioprinting has been applied in studies using bones, blood vessels, composite tissues, vascular grafts, tracheal splints, cartilaginous structures, heart tissue (e.g., two-valve heart), and vaginal organs (1).
View the full article below – Login Required
With conference presentations and other studies discussing the future of printable tissues and organs, it’s difficult not to be captivated (2). For now, current applications are focused on short-term objectives such as 3D cell cultures, technology advancement, and addressing the critical need for functional living tissues (e.g., kidney and liver) in drug discovery and preclinical screening (e.g., nephrotoxicity studies, biomimetic cellular skin substitutes). Bioprinting is founded on tissue engineering, 3D modeling technology, and digital and mechanical principles, and that knowledge base is growing and changing rapidly. With those changes in mind, biomanufacturers of tissue-based therapies will need to develop processes that will not only keep pace, but also prove to be robust and cost efficient.
Technology Components
Mechanics: Most well-funded laboratories have bioprinters solely for tissue engineering research. Although the cost of bioprinters has made them commercially feasible (US$10,000–$200,000), some universities and private corporations have specialty designed platforms. Most in vitro bioprinting technologies are based on nozzles, inkjets, or lasers. Microextrusion (fused deposition modeling) bioprinters extrude viscous liquid or molten material through a thin nozzle. Inkjet bioprinting (similar to 2D printers), uses print reservoirs and thermal or piezoelectric print heads. Stereolithography (vat photopolymerization) bioprinting uses patterned light to selectively polymerize a liquid photopolymer. Material is built on a platform surface layer by layer, and the material cures when exposed to visible or UV light (3).
One early research area is implementing laser-induced forward transfer (LIFT)-based bioprinting for in vivo repair (e.g., pilot studies with skin cells and repair of osteochondral tissues) (4). However, those studies have yet to mimic the full hierarchical structures and functions of natural tissues (e.g., sweat glands).
Inks: Bioprinters use specifically designed “inks” consisting of biomaterials, hydrogels, and living cells to build 3D tissues and organs. Much of the research in hydrogel-based bioinks involve studying the effect of ink rheology on cell viability, biocompatibility, and biofunctionality (5, 6). A common research platform (especially in academia) is the use of an extrusion printer with human mesenchymal stem cells (hMSCs), which are multipotent stromal cells that differentiate into a large range of cell types, including osteoblasts (bone cells), chondrocytes (cartilage), and myocytes (muscle).
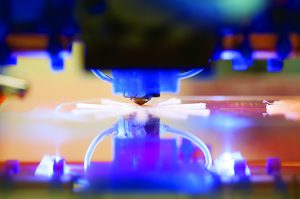
HTTPS://STOCK.ADOBE.COM
Scaffold and Nonscaffold Printing: Different approaches can be used to construct tissues. Researchers can create biocompatible templates onto which stem cells and their derivative cells can be seeded. Alternatively, decellularization (isolation of the extracellular matrix, ECM) can be used to create templates onto which researchers can seed stem cells or stem-cell–derived cells. Finally, tissues can be made directly from stem cells and matrix materials with 3D bioprinting.
Bioprinting can be performed with or without scaffolds. Scaffolds (typically made of hydrogels) encapsulate cells, allow interaction between them, and support their growth. They also can mimic the ECM environment to increase scaffold support. Scaffolds also allow for high resolution, high accuracy, and short bioprinting time (7). Complications can arise, however, if a scaffold is too soft or if it degrades too rapidly. In such a case, additional work in engineering and development would be required. Also, problems can arise when a nonbiodegradable scaffold must be removed.
Scaffold-free bioprinting (8, 9) does not involve the use of hydrogels (or other such construct materials). Instead of proliferating within a hydrogel structure, cells are “triggered” to deposit ECM components in a confined space as designed (e.g., cylinder, torus, spheroids), and the cells are allowed to fuse (7). So far, scaffold-free bioprinting can be used only with material-extrusion bioprinters. Specific cell-aggregate–based bioinks also must be developed because traditional bioink materials typically are too weak to hold complex structures. But perhaps the largest disadvantage is that the method requires using billions of cells produced by cell bioprocessing (see “Expansion of hMSCs” box and “Cell Scale-Up” below) (10).
Most experts believe that a hybrid of scaffold and scaffold-free strategies will be needed (7). For complex organs biofabrication lines might require cell sorters, cell differentiators, robotic tissue spheroids, biofabricators, robotic bioprinters, and bioreactors (9). For example, one company providing functional human tissues for drug research and screening is Organovo (San Diego, CA). The company has developed a bioprinting platform using molds to produce functional human tissues contained in standard multiwell tissue culture plates. The tissues share many key features with native tissue. After establishing a tissue design, the company develops bioprocess protocols to generate the bioink cells for target tissue. The proprietary process dispenses bioink layer by layer to a specified scale. In some cases, bioinert hydrogel components are used as supports or as fillers to create channels. The company recently launched its ExVive human liver tissue for use in toxicology and other preclinical drug testing (11).
One early stage 3D functional cellular tissue engineering construct is based on the use of perfusable chips. At Biotech Week Boston Conference (October 2016), David Kolesky (Harvard University, Wyss Institute for Biologically Inspired Engineering) discussed his research group’s work in creating three-dimensional human renal proximal tubules (PT) in vitro, fully embedded within an extracellular matrix, and housed in perfusable tissue chips. The team worked with Roche Pharmaceuticals on PT functionality protein expression and 3D printing of vascularized tissue. The enabling platform used multimaterial printing, with different inks for each type of construct (vasculature, ECM, and cellular) (12, 13).
Addressing Process Challenges
Vasculature presents a major challenge in bioprinting tissues. Blood-vessel-like channels and vascular networks are needed between layers to support cell viability, postprinting proliferation, and differentiation in terms of growth factors and gas transport (14). Early bioprinting applications were limited to creating thin avascular structures. But several studies have seen some progress in this research area (1, 12, 15–16).
Cell Scale Up: With the current pace of 3D bioprinting and the increasing number of studies requiring a large number of cells, the bioprocess industry will need to accelerate cell expansion and become much more efficient in cell processing (17). As Jordan Miller points out, “Scaling up tissue constructs is first and foremost a numbers game. Although humans are thousands of times larger than mice, human cells and mouse cells are about the same size. So to translate thin tissue studies in mice to cellularized solid-organ therapies for humans, we are going to need to be able to grow a lot more cells” (10).
But generating billions of hMSCs can take several weeks and tens of thousands of dollars. “I see bioprinting as a field of tissue engineering. For the progression of bioprinting as a technology, we need to do a lot of it — over and over,” says Jon Rowley, founder and chief technical officer of RoosterBio. The company supplies systems that enable its customers to expand the large number of cells needed quickly and cost effectively.
By mid-2016, nearly 500 MSC-based clinical trials were either complete or ongoing, according to the database of the US National Institutes of Health (18). Bioprinting addresses the critical need for functional in vitro tissue models and advanced tissue mimetic environments (19) to slow the rate of late-stage failures in clinical trials due to unsuccessful toxicity and efficacy results. “Bioprinting technologies are still relatively in their infancy,” says Rowley. “If we don’t increase the pace of the development of bioprinting as a technology, along with downstream processes and applications at the clinic, then therapies will eventually take longer and longer to reach patients.”
References
1 Yoo J. Current Developments and Clinical Perspectives of Bioprinting Technology. Biotech Week Boston: 7 October 2016.
2 Szczerba RJ. No Donor Required: 5 Body Parts You Can Make With 3-D Printers. Forbes 17 June 2015.
3 Chartrain N, Williams CB, Whittington AR. Engineering Tissues with Bioprinting. BioProcess Int. 14(10) 2016: 28–33.
4 Wang M, et al. The Trend Towards In Vivo Bioprinting. ResearchGate July 2015; doi: 10.18063/IJB.2015.01.001.
5 Chung J. Bio-Ink Properties and Printability for Extrusion Printing. Liv. Cells. Biomater. Sci. 1, 2013: 763–773; doi: 10.1039/C3BM00012E.
6 Nishiyama Y, et al. Ink Jet Three-Dimensional Digital Fabrication for Biological Tissue Manufacturing: Analysis of Alginate Microgel Beads Produced by Ink Jet Droplets for Three Dimensional Tissue Fabrication. J. Imaging Sci. Technol. 52(6) 2008.
7 Ozbolat IT. Scaffold-Based or Scaffold-Free Bioprinting: Competing or Complementing Approaches? J. Nanotechnol. Eng. Med. 6 2015; doi: 0.1115/1.4030414.
8 Norotte C, et al. Scaffold-Free Vascular Tissue Engineering Using Bioprinting. Biomaterials 30(30) 2009: 5910–5917; doi: 10.1016/j.biomaterials.2009.06.034.
9 Mironov V, Kasyanov V, Markwald RR. Organ Printing: From Bioprinter to Organ Biofabrication Line. Curr. Op. Biotechnol. 22(5) 2011: 667–673.
10 Miller JS. The Billion Cell Construct: Will ThreeDimensional Printing Get Us There? PLOS Biology June 2017; http://journals.plos.org/plosbiology/article?id=10.1371/journal. pbio.1001882.
11 Organovo’s Bioprinting Platform: Enabling 3D, Architecturally Correct, Fully Human Tissue for Drug Discovery and Transplantation. Cell and Gene Meeting: La Jolla, CA, October 2016.
12 Kolesky D. Biotech Week Boston: 4–7 October 2016.
13 Homan KA, et al. Bioprinting of 3D Convoluted Renal Proximal Tubules on Perfusable Chips. Sci. Rep. 11(6) 2016: 34845. doi: 10.1038/srep34845.
14 Yu Y, Zhang, Y, Ozbolat IT. Evaluation of Cell Viability and Functionality in Vessel-Like Bioprintable CellLaden Tubular Channels. J. Biomech. Eng. 135(9) 2013; doi:10.1115/1.4024575.
15 Kolesky D, et al. 3D Bioprinting of Vascularized, Heterogeneous Cell-Laden Tissue Constructs. Adv. Materials 26(19) 2014: 3124–3130; doi: 10.1002/adma.201305506.
16 Lee VK, et al. Creating Perfused Functional Vascular Channels Using 3D Bioprinting Technology. Biomaterials 35(28) 2014: 8092–8102.
17 Grigoryan B, Miller J. The Ambitious Future of Tissue Engineering. Democratizing Cell Technologies 3 January 2017. http://roosterbio.blogspot.com.
18 Squillaro T, Peluso G, Galderisi U. Clinical Trials with Mesenchymal Stem Cells: An Update. Cell Transplant. 25(5) 2016: 829–848.
19 Nguyen DG. Bioprinted 3D Primary Liver Tissues Allow Assessment of Organ-Level Response to Clinical Drug Induced Toxicity In Vitro. PLOS One 7 July 2016; http://dx. doi.org/10.1371/journal.pone.015867.
Maribel Rios is managing editor of BioProcess International; [email protected].
You May Also Like





