A Milestone in Macrophage-Based Cancer Treatment: Leveraging Chimeric Antigen Receptors To Address Solid TumorsA Milestone in Macrophage-Based Cancer Treatment: Leveraging Chimeric Antigen Receptors To Address Solid Tumors
The biopharmaceutical industry has reached an inflection point regarding chimeric antigen receptor (CAR) technology. CAR-bearing T cells have become an established treatment modality for hematological indications. Consider that before such products emerged in clinical and commercial contexts, children and young adults with relapsed/refractory B-cell acute lymphoblastic leukemia (R/R B-ALL) expected five-year survival rates of 21% and 10%, respectively. Today, 70–90% of B-ALL patients who are treated with CD19-directed CAR T cells can achieve complete remission (1). Since the 2017 debut of Kymriah (tisagenlecleucel) from Novartis, five other such products have received US Food and Drug Administration (FDA) approval (2). CAR-T has become a second-line treatment option in some cases (3). Drug developers recognize, however, that the modality continues to have limited efficacy against solid tumors, which represent 90% of cancers in human adults and 30% of those in children (4–6). Thus, CAR-based approaches still have much ground to traverse if the goal is to treat the largest possible patient populations.
Emboldened by currently available CAR-T products and related advances in immunological and biomanufacturing understanding, drug developers are beginning to push the CAR concept in new directions. Such work often involves research into increasingly sophisticated CAR-T designs, such as those based on “armored” T cells redirected for universal cytokine-mediated killing (TRUCKs). Because TRUCKs are designed to express transgenic cytokines, enzymes, and/or costimulatory ligands upon receptor engagement, such cells hold promise for enhancing antitumor activity (7, 8) — although that advantage still needs to be demonstrated in clinical trials. In other cases, developers are engineering new cell types for CAR expression in the hope of leveraging other immune-system functions to navigate evasive and immunosuppressive tumor microenvironments.
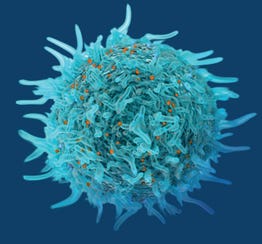
Although industry veterans might be more familiar with CAR-expressing natural killer (NK) cells, another promising permutation of the CAR concept involves genetically engineered macrophages (9–11). As this emerging modality begins to make headway in early stage clinical trials, I had the chance to speak with Michael Klichinsky, a coinventor of CAR-macrophage (CAR-M) technology and a cofounder of Carisma Therapeutics (originally Carma Therapeutics), at which he serves as chief scientific officer. He holds a PharmD degree from the University of Sciences in Philadelphia (now part of Saint Joseph’s University) and a PhD in pharmacology from the University of Pennsylvania, where he developed CAR-macrophage technology under the mentorship of Saar Gill and Carl June. During our discussion, Klichinsky highlighted clinical advantages that CAR-expressing macrophages could hold over their T-cell counterparts. He also described how recent advances in viral vectors could make CAR-Ms and related therapies viable from a manufacturing perspective.
Surmounting CAR-T Limitations
What are CAR-bearing macrophages, and why did your company begin researching such cells as therapeutics? CAR-T has treated leukemia successfully, and the modality is beginning to show promise against some lymphomas and myelomas. But solid tumors remain an intractable problem regardless of indication, target antigen, CAR design, and treatment regimen. While working in the June and Gill Laboratories at the University of Pennsylvania, we hypothesized that using macrophages could overcome some of the limitations facing CAR-T approaches in solid-tumor contexts.
Macrophages are innate immune cells. If you biopsy a solid tumor and ask which immune-cell type is most abundant in your sample, the answer is macrophages in almost every case. Tumors devote considerable energy to recruiting macrophages, whereas they generally try to exclude T cells. The reason for that is simple: T cells can recognize new antigens and thus pose a threat to tumor growth. On the other hand, macrophages can function as immunosuppressive cells when appropriately polarized to a suppressive phenotype, promoting tumor growth and immune escape.
Carisma takes a “Trojan horse” approach to cell therapy, provisioning the cells that tumors like to recruit with CARs. When a CAR-M binds with a target antigen, the cell is designed to activate as it would during typical antibody-driven immune responses: It will phagocytose the bound cancer cell, induce inflammatory cytokine release, and then present tumor-derived antigens to T cells.
CAR-T therapies have improved significantly over the past 20 years, especially because of improvements in CAR design. Why do even current generations of CAR-T therapies show limited effectiveness against solid tumors, and how could CAR-M treatments improve outcomes for patients? Drug developers have put considerable effort into increasing CAR-T potency and modulating CAR signaling to give T cells specific phenotypes — e.g., a phenotype that shows higher activation, increased durability, or decreased susceptibility to T-cell exhaustion. Such advances are irrelevant if administered CAR T cells fail to reach a tumor in a sufficient quantity. If they do not enter a tumor and bind their target antigens, then it won’t matter how souped up the CAR is.
Other obstacles come from the many forms of immunosuppression that solid tumors leverage. When properly activated and expanded, T cells perform some of the fastest divisions known in biology. But speedy division requires considerable nutrients, oxygen, and other resources — not to mention conditions such as appropriate blood flow. Tumors simply lack such resources. Cancer cells also produce a host of immunosuppressive factors — including interleukin 10 (IL-10), transforming growth factor β (TGF-β), and programmed–cell-death receptor ligand 1 (PD-L1) — to hasten T-cell exhaustion.
A third, often overlooked factor is that CAR-T usually has succeeded in the context of CD19-targeted therapies. CD19 is a highly expressed antigen that presents on nearly all B cells and B-cell cancers. But target-antigen expression is extremely heterogeneous in solid tumors. Some tumor cells express the antigen in varying quantities; other such cells do not present the antigen at all. Solid tumors effectively modulate antigen expression levels to their advantage. Let’s imagine that 20% of a patient’s tumor cells express that target antigen. The best-case scenario, then, is that CAR-T therapy kills all of those cells. But within a few weeks, the remaining 80% of tumor cells — which are inherently resistant because they do not bear the target antigen — will continue growing. Then, the tumor will be almost completely resistant to that targeted therapy.
Macrophages raise several advantages by comparison. Such cells can access tumors easily because they express different receptors and engage in distinct trafficking pathways. Some macrophages are unaffected by the immunosuppression strategies that diminish CAR-T efficacy in tumor microenvironments. Macrophages are phenotypically plastic. For simplicity’s sake, let’s say that they can assume one of two polarization states: M1 or M2. M1-state macrophages can maintain inflammatory pressure on tumor cells even in an immunosuppressive environment. Thus, at Carisma Therapeutics, we lock our CAR-Ms into the M1 phenotype.
Developers of CAR-T products cannot get around the problem of antigen heterogeneity because a CAR can target only one antigen. However, for CAR-M therapies, the receptor simply functions as a foothold — something to get phagocytosis going and initiate the cycle. Then, because macrophages are professional antigen-presenting cells (APCs), they will present tumor-specific neoantigens for other immune cells to recognize and destroy. Consider a cancer patient whose tumors show KRAS protooncogene mutations and overexpress human epidermal growth factor receptor 2 (HER2). Anti-HER2 CAR-M binding will lead to HER2-dependent phagocytosis, but then that macrophage will present the KRAS mutation to T cells, which in turn can attack tumor cells that do and do not express the initial CAR target. That process, called epitope spreading, is critical to the success of any immunotherapy for solid-tumor indications. T and NK cells are not APCs, so they cannot process or present antigens directly. Only monocytes, macrophages, and dendritic cells have that function.
How much attention have macrophage-based therapies received from researchers and drug developers? Is the macrophage field still quite nascent? Our company was the first to work with CAR-M therapies. Over the past couple of years, though, the field has started to grow exponentially. Judging from the number of articles about CAR-macrophages on PubMed, we might say that the field has reached the same point as CAR-T did maybe 10 years ago.
Many studies have focused on genetically unmodified macrophages. German hematologist Reinhard Andreesen performed initial experiments in the 1990s (12). His hypothesis was that, because macrophages are phagocytic cells, they could (without modification) take up cocultured bacteria, limiting colony formation in the culture vessel. Subsequent studies showed that macrophages activated with cytokines could phagocytose cancer cells, such that those cells showed a diminished growth rate.
With that early concept, developers took autologous monocyte-derived macrophages into the clinic studies, which demonstrated the safety of macrophage therapy (13). In some cases, cells trafficked to tumors, achieving mild improvement in ascites for patients with peritoneal carcinomatosis (a complication of ovarian cancer in the peritoneal cavity), but did little to diminish tumor growth substantially. Trial outcomes were lackluster because macrophages need a way to recognize a tumor as a target. Moreover, simply readministering macrophages to a patient does not enable the cells to attack a tumor; they need to be polarized in the M1 direction or else the tumor will recruit the cells to become immunosuppressive.
Our CAR-M concept is meant to overcome both of those limitations. A CAR is essentially a sense-and-response system. The receptor binds to a target antigen (e.g., HER2) and emits a signal to activate a cascade that leads to further immune-cell activation and killing of cancer cells. We also polarize the cells to the M1 phenotype so that tumors cannot make them immunosuppressive.
A natural question to ask is, why did it take so long to put CARs on macrophages? Such cells are difficult to modify genetically. The vectors that are used to produce CAR T and NK cells — lentiviruses and retroviruses — simply do not work on human macrophages. Being RNA viruses, lentivirus and retrovirus release RNA genomes into infected cells. That material needs to be reverse-transcribed into DNA and then get integrated into a host cell’s genome. Reverse transcription requires that cells have DNA nucleotides available. But because macrophages actively suppress their pools of free nucleotides, reverse transcription cannot take place. Thus, lentivirus and retrovirus can enter macrophages but cannot convert their RNA genomes into DNA genomes.
As a graduate student, I researched gene delivery into macrophages. Our team found a robust way to accomplish that using an engineered adenoviral (Ad) vector called Ad5.F35 (9). It is designed to express chimeric fiber proteins comprising the knob and shaft of Ad serotype 35 (Ad35) and the fiber tail of Ad serotype 5 (14, 15). Ad5.F35 vectors can transduce human macrophages and monocytes with high efficiency. Our laboratory at Carisma routinely observes >90% CAR expression and high macrophage viability after Ad5.F35 transduction, whereas researchers typically observe <5% CAR expression when using lentiviruses and retroviruses. Identifying the Ad5.F35 vector was one of the key findings that enabled the development of CAR-M therapy.
Making Clinical Headway
How would you describe your company’s CT-0508 candidate? How does it leverage the immunological advantages of macrophages that you mentioned earlier? CT-0508 is the first CAR-macrophage treatment to enter human clinical trials. It is an autologous monocyte-derived macrophage engineered with Ad5.F35 to express an anti-HER2 CAR. The candidate is undergoing a phase 1 safety study as a monotherapy (16). In a distinct substudy, clinicians also are evaluating the therapy in combination with pembrolizumab, a T-cell checkpoint inhibitor (17). The trial is treating patients with HER2-overexpressing solid tumors. The format is a basket trial, so it is not limited to a particular disease. But among 14 patients for whom we have presented data publicly, about half of our subjects have breast cancer, and the other half have gastroesophageal cancers, as we would expect in the HER2 space.
CT-0508 has a few key characteristics. It is M1 polarized. Early evaluations showed that macrophages from all patients took on that proinflammatory phenotype by the end of manufacturing. We also analyzed manufactured CAR-macrophages from each patient to assess key functionality requirements — e.g., the abilities to phagocytose HER2-positive tumor cells and produce inflammatory cytokines. Results from those experiments showed that manufactured CAR-macrophages were functional in all patient lots.
Feasibility and functionality were key parameters going into the clinical phase. Trial subjects have extremely advanced diseases. Patients in our study have undergone five to 12 prior lines of treatment. All have undergone multiple rounds of chemotherapy; others have also had radiation; and all of them have received HER2-targeted therapies such as monoclonal antibodies (mAbs) and antibody–drug conjugates (ADCs). The big question, then, was whether patients’ myeloid cells were too beaten up to be manufactured into effective CAR-Ms. But the autologous macrophages worked. Cells resulting from our process showed the right phenotype, were produced in sufficient quantities, and exhibited properties that made them indistinguishable from CAR-Ms made from healthy-donor material.
In our current first-in-human (FiH) study, safety is the focus. So far, CT-0508’s safety profile has been quite good. When you think about CAR-T therapeutics, you worry about severe cytokine release syndrome (CRS) and neurotoxicity, both of which have earned black-box warnings for marketed products. To date, the CT-0508 candidate has not triggered severe CRS. Trial subjects sometimes have experienced mild (grades 1 and 2), self-limiting CRS, but no severe illness (grades 3 and 4) has occurred. We have observed no neurotoxicity. Overall, the candidate has been well tolerated. A related factor is that therapies based on CAR T cells, CAR NK cells, tumor-infiltrating lymphocytes (TILs), and T-cell receptors (TCRs) all require lymphodepletion. We do not believe that such procedures are necessary before CAR-M administration — a unique feature among gene-modified cell therapies that enhances our candidate’s safety profile.
In terms of efficacy, we knew from preclinical studies that CT-0508 should be studied in a combination regimen. CAR-Ms have direct antitumor activity, but a significant part of the CAR-macrophage mechanism of action (MoA) derives from its propagation of epitope spreading, which further activates T cells. In late-stage solid tumors, T cells already are experiencing exhaustion. We believe that a combination regimen with a CAR-macrophage therapy and a checkpoint inhibitor could help to overcome that limitation. Although pembrolizumab and other anti-PD-1/PD-L1 drugs have been immensely successful, most patients do not respond to monotherapy. Our goal is to use CAR-macrophages to convert nonresponding cells into responders.
Thus far, the best overall response achieved in our monotherapy trial has been stable disease, which we observed in 28% of subjects. Using single-cell analysis, we evaluated the candidate’s MoA in patient biopsy material. As was the case during preclinical studies in animals, we found that CT-0508 activated the tumor microenvironment, recruited T cells, increased intratumoral inflammation, and induced antitumor responses from T cells. At the same time, we noticed a high level of T-cell exhaustion that increased during treatment. When you activate T cells, you also induce protective inhibitory pathways such as that for PD-1. Ultimately, the monotherapy trial has demonstrated the safety of CAR-M approaches and validated the MoA. Both the monotherapy and combination trials are ongoing.
Manufacturing Matters
What is a typical workflow for CAR-macrophage production? First, patients receive a subcutaneous injection of filgrastim, a recombinant granulocyte colony-stimulating factor (G-CSF) that increases peripheral-blood monocyte counts. As with autologous CAR-T products, patients undergo apheresis to extract blood, which is shipped to a manufacturing site. (Novartis performs this step for our CT-0508 candidate at one of its New Jersey facilities). Then, we use a CliniMACS Prodigy instrument (Miltenyi Biotec) to isolate monocytes from the leukopak material, perform a purification step, and differentiate the purified cells into macrophages. Then, as we discussed, Ad5.F35 vectors are used to transduce the macrophages. That step has a dual effect, delivering gene sequences for CAR expression while polarizing the macrophages into an M1 phenotype. Ultimately, manufactured cells are washed, processed, and cryopreserved until thawing and intravenous administration.
The whole process takes about a week from blood draw to product cryopreservation. The vein-to-vein time is a bit longer than that because of quality control (QC) steps that are standard for autologous cell therapies — e.g., testing for sterility, mycoplasma, and endotoxins. Thus, vein-to-vein time is three to four weeks.
How might vein-to-vein times be decreased? One option involves the monocyte-differentiation step. In November 2023, we announced investigational new drug (IND) clearance for our CT-0525 candidate, which leverages monocytes rather than monocyte-derived macrophages. CT-0525 is undergoing a phase 1 clinical study. We have found that monocytes present some advantages over macrophages. CAR-bearing monocytes still become CAR-macrophages, but rather than performing a differentiation step ex vivo, we can administer CAR-monocytes to patients and have the cells differentiate there.
Having manufactured cells differentiate in vivo shortens the production process from one week to about one day. That strategy also enables us to produce fivefold more cells than we could in a CAR-macrophage process. We believe that dosing matters to therapy efficacy. On average, we can produce about 2 billion CAR-macrophages per patient, but with CAR-monocytes, we could produce up to 10 billion cells, enabling patients to receive higher doses.
Monocytes also raise several pharmacologic benefits. Preclinical studies have shown that monocytes traffic into tumors more readily, persist long after administration, and exhibit greater potency than do macrophages. We have yet to share data about the candidate, but the CT-0525 candidate is essentially a next-generation approach to the CT-0508 CAR-M.
The Future of Macrophage Therapy
You mentioned monocytes’ advantages for production capacity. Compared with other CAR modalities, how scalable might processes for CAR-bearing macrophages and monocytes be? The industry needs to address that question soon because the solid-tumor patient population is considerably larger than are those for leukemia, lymphoma, and myeloma. Consider that the number of breast cancer patients in the United States is higher than it is for all hematologic malignancies. That said, developers still are working on bringing CAR cell therapies to the solid-tumor space. To date, no CAR-based therapy has received regulatory approval for a solid-tumor indication.
Nevertheless, the field is growing, with exciting technologies emerging to facilitate scale-up. Several companies are developing innovative automation technologies for custom cell-therapy processes. From our point of view, the CT-0525 CAR-monocyte manufacturing process is about as streamlined as an autologous workflow can get because our systems are fully automated and closed.
It is worth mentioning that Carisma entered into a collaboration with Moderna about two years ago (18). The idea was to leverage Moderna’s lipid nanoparticle (LNP)–encapsulated mRNA technology to generate CAR-macrophages in vivo rather than manufacturing a cell therapy that undergoes manipulation outside a patient’s body. Moderna has developed an LNP that is particularly successful in transfecting macrophages in the body.
From a scalability perspective, an off-the-shelf, LNP-encapsulated therapeutic would be ideal. It could be manufactured at large scales, and because it would work directly within a patient’s body, it could overcome many of the complexities associated with ex vivo cell therapy. At the November 2023 Society for Immunotherapy of Cancer (SITC) meeting, Carisma presented data showing that such a strategy works in animal models and a variety of tumor models (19). We also announced the selection of our first lead candidate under the collaboration, and the program continues to move toward IND-enabling studies (20).
References
1 Xu X, et al. Mechanisms of Relapse After CD19 CAR T-Cell Therapy for Acute Lymphoblastic Leukemia and Its Prevention and Treatment Strategies. Front. Immunol. 10, 2019: 2664; https://doi.org/10.3389/fimmu.2019.02664.
2 Approved Cellular and Gene Therapy Products. US Food and Drug Administration: Silver Spring, MD, 2024; https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/approved-cellular-and-gene-therapy-products.
3 Lutfi F, et al. Second-Line Treatment with CAR T-Cell Therapy for Large B-cell Lymphoma. Clin. Adv. Hematol. Oncol. 21(4) 2023: 170–178; https://pubmed.ncbi.nlm.nih.gov/37039724.
4 Mitra A, et al. From Bench to Bedside: The History and Progress of CAR T Cell Therapy. Front. Immunol. 14, 2023; https://doi.org/10.3389/fimmu.2023.1188049.
5 Dejenie TA, et al. Current Updates on Generations, Approvals, and Clinical Trials of CAR T-Cell Therapy. Hum. Vacc. Immunother. 18(6) 2022: 2114254; https://doi.org/10.1080/21645515.2022.2114254.
6 Tokarew N, et al. Teaching an Old Dog New Tricks: Next-Generation CAR T Cells. Brit. J. Cancer 120(1) 2019: 26–37; https://doi.org/10.1038/s41416-018-0325-1.
7 Chmielewski M, Abken H. TRUCKs: The Fourth Generation of CARs. Exp. Opin. Biol. Ther. 15(8) 2015: 1145–1154; https://doi.org/10.1517/14712598.2015.1046430.
8 Glienke W, et al. GMP-Compliant Manufacturing of TRUCKs: CAR T Cells Targeting GD2 and Releasing Inducible IL-18. Front. Immunol. 13, 2022; https://doi.org/10.3389/fimmu.2022.839783.
9 Klichinsky M, et al. Human Chimeric Antigen Receptor Macrophages for Cancer Immunotherapy. Nature Biotechnol. 38(8) 2020: 947–953; https://doi.org/10.1038/s41587-020-0462-y.
10 Pan K, et al. CAR Race to Cancer Immunotherapy: From CAR T, CAR NK, to CAR Macrophage Therapy. J. Experim. Clin. Cancer Res. 41(119) 2022; https://doi.org/10.1186/s13046-022-02327-z.
11 Niu Z, et al. Chimeric Antigen Receptor-Modified Macrophages Trigger Systemic Anti-Tumour Immunity. J. Pathol. 253(3) 2021: 247–257; https://doi.org/10.1002/path.5585.
12 Andreesen R, Hennemann B, Krause SW. Adoptive Immunotherapy of Cancer Using Monocyte-Derived Macrophages: Rationale, Current Status, and Perspectives. J. Leukocyte Biol. 64(4) 1998: 419–426; https://doi.org/10.1002/jlb.64.4.419.
13 Moroni F, et al. Safety Profile of Autologous Macrophage Therapy for Liver Cirrhosis. Nat. Med. 25(10) 2019: 1560–1565; https://doi.org/10.1038/s41591-019-0599-8.
14 Flickinger JC Jr., et al. Chimeric
Ad5.F35 Vector Evades Anti-Adenovirus Serotype 5 Neutralization Opposing GUCY2C-Targeted Antitumor Immunity. J. Immunother. Cancer 8(2) 2020: e001046; https://doi.org/10.1136/jitc-2020-001046.
15 Chen S, et al. Harnessing and Enhancing Macrophage Phagocytosis for Cancer Therapy. Front. Immunol. 12, 2021; https://doi.org/10.3389/fimmu.2021.635173.
16 CT-0508 Study. Carisma Therapeutics: Philadelphia, PA, 2024; https://www.her2macrophagetrial.com/about-the-study.
17 CT-0508 in Combination with Pembrolizumab Substudy. Carisma Therapeutics: Philadelphia, PA, 2024; https://www.her2macrophagetrial.com/pembrolizumab-combo-study.
18 Moderna and Carisma Establish Collaboration To Develop In Vivo Engineered Chimeric Antigen Receptor Monocytes (CAR-M) for Oncology (press release). Moderna Therapeutics: Cambridge, MA, 10 January 2022; https://investors.modernatx.com/news/news-details/2022/Moderna-and-Carisma-Establish-Collaboration-to-Develop-in-vivo-Engineered-Chimeric-Antigen-Receptor-Monocytes-CAR-M-for-Oncology/default.aspx.
19 Carisma To Present First Results From In Vivo CAR-M Collaboration with Moderna at SITC 2023 (press release). Carisma Therapeutics: Philadelphia, PA, 25 October 2023; https://ir.carismatx.com/news-releases/news-release-details/carisma-present-first-results-vivo-car-m-collaboration-moderna.
20 First In Vivo CAR-M Lead Candidate Nominated Under Carisma–Moderna Collaboration (press release). Carisma Therapeutics: Philadelphia, PA, 14 December 2023; https://ir.carismatx.com/news-releases/news-release-details/first-vivo-car-m-lead-candidate-nominated-under-carisma-moderna.
Brian Gazaille, PhD, is managing editor of BioProcess International, part of Informa Connect Life Sciences; [email protected].
Please email [email protected] to speak with Carisma Therapeutics about CAR-macrophage and CAR-monocyte therapies.
You May Also Like






