The Delivery Dilemma: Looking Beyond Viral Vectors for Gene TherapyThe Delivery Dilemma: Looking Beyond Viral Vectors for Gene Therapy
October 15, 2024
The term gene therapy (GT) encompasses a range of strategies for modifying or influencing genetic information either to treat or to prevent disease. GTs include both systems that work by introducing, replacing, or altering the existing genetic material within a patient’s cells — often called gene-modified cell therapy when performed ex vivo — and those that use genetic material to influence or modulate the in vivo expression of genes. Probably for mechanistic reasons, other emerging therapies such as viral oncolytics sometimes are included in GT discussions. It’s helpful to understand that categorical statements regarding many aspects of GT can be difficult because of exceptions to some stated generalities about components and desired functions.
Some GTs involve genetic engineering systems as clustered regularly interspaced short palindromic repeats (CRISPR) and CRISPR-associated protein 9 (Cas9). The combination provides a powerful gene-editing tool for precise and permanent modification of DNA sequences within cells. Oligonucleotide therapy, alternatively, delivers short DNA or RNA sequences (oligos) that generally modulate gene expression or correct a patient’s abnormal RNA function. Such products include antisense oligos (ASOs), small interfering RNA (siRNA), messenger RNA (mRNA), and others.
There are two basic approaches to GT: in vivo and ex vivo therapies. In vivo GT introduces genetic or gene-altering materials directly into a patient’s body, with the therapeutic effect thus occurring within a living organism. In ex vivo GTs, patient or donor cells are collected, genetically modified in culture, often expanded in numbers, and then reintroduced into a patient (autologous therapy) or patients (allogeneic therapy).
Viral vectors — e.g., adenovirus vectors (AdVs), adeno associated virus vectors (AAVs), and lentivirus vectors (LVVs) such as human immunodeficiency virus (HIV) — have proved to be the most GT popular delivery agents to date. They play a crucial role in packaging, protecting, stabilizing, and delivering gene-altering materials into cells (1, 2). That said, other delivery methods are under exploration and development. Researchers are interested in identifying specific features (new advantages) and incremental benefits over viral vectors and alleviating known limitations of existing viral delivery methods. One advantage to nonviral vectors (NVVs) is their relative safety due to the absence of immunogenic viral proteins.
Viral-Vector Concerns
Viral vectors can evoke immune responses in recipients, creating safety concerns. For example, viral-vectored GTs can be immunogenic when administered to individuals who have preexisting immunity to the specific type of virus used. An immunological response upon initial dosing could limit treatment effectiveness or, worse, endanger the patient. Viral-vectored products also can be immunostimulatory, inducing a response upon first administration that obviates their future use. In such cases, patients cannot receive the same product again (or others that use the same viral vector) in the future.
In some systems, integration of viral DNA into the host genome might disrupt normal gene expression — e.g., through insertional mutagenesis — and even mediate disease (3). Although vector viruses are engineered to be replication deficient, a slight risk of recombination remains and could result in undesired viral replication. Achieving specific targeting of viral vectors to desired tissues or cells can be difficult, and each virus has its own limitations in capacity for carrying large genes or therapeutic payloads. Some experts are concerned especially about the potential of low frequency, late-onset side effects (1). And some concern remains regarding the spread of payloads to unintended tissues or organs — and even the potential for horizontal gene transfer to other organisms.
In terms of design and customization to particular applications, viral vectors can be limited in flexibility and available options. Many researchers prefer to tailor drug-delivery systems to specific cargoes, therapeutic needs, and target cell types. When the delivery agent is a closed viral system, that can limit the adjustment of some parameters (e.g., inserted oligonucleotide size). Depending on the vector and type of GT being considered, viral genetic material could be introduced into a host genome in a nonengineered way, which raises concerns about insertional mutagenesis. NVVs lack the machinery to affect the integration of unintended genetic material into a host genome, which reduces the risk of potentially dangerous genetic alterations.
Producing viral vectors at scale with consistent quality is complex and costly, posing challenges for widespread therapeutic use. It involves complex biological systems, including cell cultures and viral replication cycles that require precise conditions to ensure vector stability and functionality (4). Maintaining consistency and purity across batches of viral vectors is difficult, especially considering the risk of contamination by other viruses, mycoplasma, and unwanted cellular byproducts. Viral-vector production is labor intensive, and volumetric yields can be low, especially for lenti- and retroviruses. Scaling up can be quite complex and inflexible.
Benefits of Nonviral Vectors
My interest in delivery vectors began in the late 1970s while I was working in the laboratory of Demetrios Papahadjopoulos at Roswell Park Memorial Institute in Buffalo, NY. At the time, he was showing that liposomes could deliver entrapped drugs and vaccines to cells and thus eliminate some problems related to “raw” drug dosing. It wasn’t long before the idea arose for using liposomes to deliver DNA, which since then has culminated in the current idea of using such synthetic vesicles in GT and genetic immunization. All GT cargo carriers, including viral vectors, play a crucial role in protecting, stabilizing, and delivering genetic material to target cells.
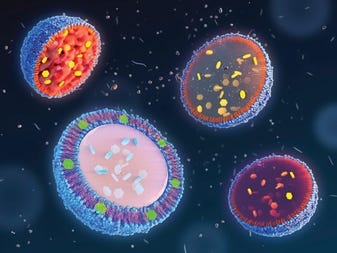
Many different approaches now are in development for nonviral (mostly synthetic) delivery of cargo to treat genetic and acquired disorders with GT (5). A renowned example of in vivo therapy using a nonviral delivery vector is mRNA COVID-19 vaccine technology. The SARS-CoV-2 spike protein is encoded in mRNA encapsulated within lipid nanoparticles (LNPs), which create a lipid bilayer to protect fragile mRNA from degradation and facilitate its functional delivery into recipients’ cells. Those cells then express the encoded protein, which induces a prophylactic immune response.
With respect to the risk of immediate adverse immune reactions, NVVs typically are safer and less immunostimulatory than viral vectors. And as for vector flexibility, some NVVs can accommodate aspects of vector design, targeting, and customization to particular applications that are not possible with viral systems. Some researchers tailor lipid or polymeric nanoparticles (as well as other NVVs) to suit specific nucleic-acid cargoes, therapeutic needs, and target cell types. And some NVVs have the capacity for larger payloads than viral vectors can carry. That can support delivery of larger oligonucleotide sequences and even multiple therapeutic agents at once, making NVVs suitable for delivering complex therapeutic payloads.
More versatile NVVs can be used to develop platforms for delivering an array of nucleic acids. Such adaptability enables NVV developers to design approaches for a range of GT initiatives. Engineering to enhance tissue targeting and specificity is a current concern for many GT programs. NVVs often can provide a breadth of possibilities for improving the precision of gene delivery to desired tissue or cell types. Such methods have been investigated for both in vitro and in vivo applications, with some more advanced for one than the other.
Note that scale considerations can constitute a significant factor in viral-vector manufacturing. Some NVVs are easier and less expensive to transfer into production and manufacture at scale by comparison. That facility can reduce the cost of at-scale manufacturing — savings that could help to reduce costs for payers and patients — while improving the effectiveness of GT treatments.
So the advantages of nonviral vectors include reduced risk of inflammation, toxicity, and other immune-related complications (5, 6). Because they elicit lower immune responses, most can be administered multiple times without losing effectiveness, which is especially beneficial for chronic conditions that require ongoing treatment. NVVs — especially those made from biodegradable materials — present a reduced risk of insertional mutagenesis and can be less toxic. Chemically based vectors are typically easier and less expensive to produce at large scale compared to viral vectors, often with less variation between batches. Nonviral vectors can be designed with specific targeting ligands that enhance delivery to specific tissues or cell types, thus improving therapeutic efficacy and making them less likely to affect unintended tissues or organs.
Nonviral Technologies in Development
A number of nonviral vector systems are in different stages of development. These include virus-like particles (VLPs), lipid nanoparticles (LNPs), exosomes, polysaccharide macromolecules, cell-penetrating peptides (CPPs), inorganic nanoparticles, electroporation technologies, ultrasound methods, and polymer hydrogels (7–10).
VLPs are noninfectious particles that mimic the structure of viruses but lack any viral genetic material. They can be engineered to carry and deliver therapeutic nucleic acids. Possible approaches to producing VLPs include mammalian, yeast, insect cell, bacterial, and plant cell-based expression systems.
LNPs currently are the most popular alternative to viral vectors. Lipid structures of about 20–200 nm in diameter can serve as carriers or delivery vectors for nucleic acids such as mRNA, siRNA, and other oligonucleotides. Other related nanoparticles made from biocompatible polymers such as polyethylenimine (PEI) and poly(lactic-co-glycolic acid) (PLGA), and also can be used for nucleic-acid delivery.
Exosomes are naturally occurring extracellular vesicles with a lipid bilayer structures by which they encapsulate and protect biomolecules within them. Exosomes can be engineered to carry many different types of cargo and show reduced immunogenicity compared with LNPs and VLPs. The precision and efficiency of gene delivery is promoted by an ability to display specific targeting molecules on the exosome surface. These structures are relatively stable and have the ability to permeate such thresholds as the blood–brain barrier.
Exosomes can present many advantages over other vector options (11). Being naturally derived from cells makes them inherently biocompatible and less likely to trigger an immune response or cause cytotoxicity. Because the biomimetic membrane composition of even engineered exosomes resembles that of target cells, the exosomes can fuse with recipient cells efficiently, which facilitates uptake and delivery of their cargo. They can be engineered to express specific surface proteins or ligands that enable targeted delivery to particular cell types or tissues. Exosomes tend to be more stable in circulation than many other vectors, protecting their cargo from degradation by enzymes. They can carry a variety of biological molecules — proteins, RNA (such as mRNA, miRNA, siRNA), and DNA — without affecting a recipient’s genome.
Polysaccharide macromolecules such as chitosan and cyclodextrin are promising for their biocompatibility, enhanced cellular uptake, and versatility. Highly branched poly(β-amino esters) (HPAEs) offer versatility in synthesis, biocompatibility, and an ability to be functionalized with targeting ligands such as antibodies or peptides to improve the specificity of drug delivery.
Cell-Penetrating Peptides (CPPs) are short sequences of amino acids that have the ability to cross cell membranes and facilitate the delivery of various cargos (12). They have shown promise in delivering small molecules, proteins, nucleic acids, and nanoparticles. CPPs typically enter cells through endocytosis or direct translocation across membranes. Depending on their design and the nature of their cargo, CPPs can release cargo in either the cytoplasm or in specific organelles. A versatile tool for drug delivery that is less toxic than other options, CPPs can be modified to target specific cell types or tissues. However, they are susceptible to degradation (e.g., by proteases), which limits their effectiveness and could lead to toxicity or limited target specificity. Some CPPs have been observed to accumulate in endosomes, limiting cytoplasmic delivery.
Inorganic Nanoparticles: Jet-injection devices and “gene guns” are physical (nonchemical) methods for delivering nucleic acids directly into living tissue. Jet injection forces high-pressure streams of oligo-containing buffers directly into tissue. Gene guns use high-velocity particles such as porous platinum pellets and carbon nanotubes to deliver their genetic cargo.
These more “mechanical” methods of gene delivery derive some distinct advantages from not being biologically directed mechanisms (13, 14). However, they do demonstrate some significant limitations, especially in therapeutic application. For example, they lack precision in targeting specific cell types and can cause significant damage to the target cells or tissue. They can also exhibit inconsistent delivery efficiency and have more limited cargo capacity compared with other options. The depth of penetration into tissue is limited for particles and globules, which restricts the use of such methods to tissue surfaces and cell monolayers.
Electroporation applies electric pulses to create temporary pores or small holes in cell membranes. Simply formulated oligos then can enter the cells through those openings.
Ultrasound can be used alternatively to enhance the permeability of cell membranes for nucleic-acid delivery. This is one of the most noninvasive NVV options and has been investigated for both in vitro and in vivo applications.
Hydrogels are three-dimensional (3D) networks of hydrophilic polymers that carry buffers and genetic cargo. These structures can be designed for controlled release of nucleic acids and offer particular utility for localized in vivo delivery.
Many Means to an End
GT research is ongoing as NVV alternatives to viral vectors are continually refined and improved. The choice of delivery method for a given product will depend on factors such as the specific therapeutic application, target cells, and biophysical/biochemical characteristics of the nucleic acids to be delivered.
Over a dozen GT products have been approved so far to treat both genetic and acquired diseases — and clinical trials continue to be initiated for new product candidates. Some type of vector will be required to focus and deliver every GT cargo to target cells, whether in vivo or ex vivo. Engineered viruses currently comprise the majority of vectors in use, but they each have limitations. Developers have many diverse GT delivery tools to consider that could provide relief from those limitations, or provide additional benefit, with cost and scale benefits coming as potential and welcome side effects.
References
1 Lundstrom K. Viral Vectors in Gene Therapy: Where Do We Stand in 2023? Viruses 15(3) 2023: 698; https://doi.org/10.3390/v15030698.
2 Zhao Z, Anselmo AC, Mitragotri S. Viral Vector-Based Gene Therapies in the Clinic. Bioeng. Transl. Med. 7(1) 2022: e10258; https://doi.org/10.1002%2Fbtm2.10258.
3 Kumar SRP, Duan D, Herzog RW. Immune Responses to Muscle-Directed Adeno-Associated Viral Gene Transfer in Clinical Studies. Human Gene Ther. 34 (9–10) 2023; https://doi.org/10.1089/hum.2023.056.
4 Jiang Z, et al. Challenges in Scaling Up AAV-Based Gene Therapy Manufacturing. Trends Biotechnol. 41(10) 2023; 1268–1281; https://www.cell.com/trends/biotechnology/fulltext/S0167-7799(23)00123-3.
5 Wang C, et al. Emerging Non-Viral Vectors for Gene Delivery. J. Nanobiotechnol. 21(1) 2023: 272; https://doi.org/10.1186/s12951-023-02044-5.
6 Dogbey DM, et al. Technological Advances in the Use of Viral and Non-Viral Vectors for Delivering Genetic and Non-Genetic Cargos for Cancer Therapy. Drug Deliv. Transl. Res. 13, 2023: 2719–2738; https://doi.org/10.1007/s13346-023-01362-3.
7 Ledesma-Feliciano C, et al. Improved DNA Vaccine Delivery with Needle-Free Injection Systems. Vaccines 11(2) 2023: 280; https://doi.org/10.3390/vaccines11020280.
8 Lemprière S. Ultrasound Lets Gene Therapy into the Brain. Nat. Rev. Neurol. 19(6) 2023: 326; https://doi.org/10.1038/s41582-023-00816-z.
9 Sharma V, Mukhopadhyay CD. Exosome As Drug Delivery System: Current Advancements. Extracell. Vesicle 3, 2024: 100032; https://doi.org/10.1016/j.vesic.2023.100032.
10 Nam SH, Park J, Koo H. Recent Advances in Selective and Targeted Drug/Gene Delivery Systems Using Cell-Penetrating Peptides. Arch. Pharm. Res. 46, 2023: 18–34; https://doi.org/10.1007/s12272-022-01425-y.
11 Koh HB, et al. Exosome-Based Drug Delivery: Translation from Bench to Clinic. Pharmaceutics 15(8) 2023: 2042; https://doi.org/10.3390/pharmaceutics15082042.
12 Sun Z, et al. Cell-Penetrating Peptide-Based Delivery of Macromolecular Drugs: Development, Strategies, and Progress. Biomedicines 11, 2023: 1971; https://doi.org/10.3390/biomedicines11071971.
13 Oelkrug C. Analysis of Physical and Biological Delivery Systems for DNA Cancer Vaccines and Their Translation to Clinical Development. Clin. Exp. Vacc. Res. 13(2) 2024: 73–82; https://doi.org/10.7774/cevr.2024.13.2.73.
14 Shchaslyvyi AY, et al. Current State of Human Gene Therapy: Approved Products and Vectors. Pharmaceuticals 16, 2023: 1416; https://doi.org/10.3390/ph16101416.
BPI editorial advisor William Whitford is an independent consultant based in Logan, UT, who most recently served as life-sciences strategic solutions leader at Arcadis and can be reached at [email protected].
You May Also Like






